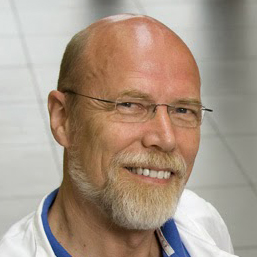
September 24, 1951- January 17, 2022
Dr. Ronald Tompkins’s work in the genomics, proteomics, and ultrastructural roles in inflammation and metabolism, and his leadership in multidisciplinary, multi-institutional large research projects energized OMF’s efforts to ignite Myalgic Encephalomyelitis / Chronic Fatigue Syndrome (ME / CFS) research across the globe. He served as OMF’s Chief Medical Officer and Co-Director of the Harvard ME/CFS Collaborative Research Center at Harvard Affiliated Hospitals.
Dr. Tompkins was widely recognized for his work in translational science, medicine, and engineering. He graduated from Tulane University in 1972 and Tulane School of Medicine in 1976. During his training in surgery at the MGH, Dr. Tompkins earned a Doctorate in chemical engineering at Massachusetts Institute of Technology (MIT). He completed his Harvard surgery residency and joined the surgical faculty at MGH in 1987. He served as Chief of Trauma and Burn Services at the MGH and Chief of Staff at the Boston’s Shriners Hospital for 22 years.
Dr. Tompkins led a fundamental and clinical research program that began in 1990, with an NIH-supported first-in-the-nation Specialized Research Center in trauma. Its associated Trauma Research Training Program produced dozens of the current leaders in the clinical and research field of injury. In 2001, he led a large-scale Collaborative Research Program in injury research, which was the largest NIH-funded program ever received by MGH and the 10th largest NIH extramural program to date nationally. These programs – with well more than $200M in public funding – provided Dr. Tompkins with a unique understanding of inflammation and metabolic features of humans in response to severe stresses.
Following these decades of significant clinical and basic science discovery, Dr. Tompkins founded a center for research and innovation, which translated scientific applications into multiple inventions and companies. Three previous companies eventually sold for a total of more than $1.2B. He served on the Boards of Directors of start-up companies in a vast array of medical applications involving Treatment for Alzheimer’s Disease, Point-of-Care Diagnostics, Chimeric Antigen Receptor (CAR) T-cell Therapies, Microcirculatory Dysfunction in the Critically Ill, and Novel Approaches to Cellular Function Ex Vivo.
Dr. Tompkins served on dozens of Scientific, Not-for-Profit, and Academic Boards and National Committees and published more than 500 research contributions in medicine and engineering journals toward the advancement of science and engineering in medicine. He delivered over 500 invited keynote and scientific meeting presentations and lectures. He received numerous honors and awards.
Learn more about Dr. Tompkins’ life and legacy.